Understanding cardiovascular disease

Cardiovascular diseases (CVD) refer to a group of heart and blood vessel disorders that are caused by atheroma (the fatty material which deposits in the arteries). It can increase the risk for heart attack, heart failure and stroke, thus resulting in decreased quality of life and decreased life expectancy. The silent killer – Hypertension (high blood pressure), is a leading risk factor for cardiovascular disease.
Know what atheroma is
Patches of atheroma are small fatty lumps that develop within the inside lining of the arteries or blood vessels. It is also known as hardening of the arteries. Over months or years, patches of atheroma (plaques) can become larger and thicker, making an artery narrower, thereby reducing the blood flow through the artery.
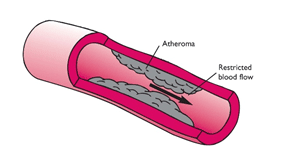
Angina for example, is narrowing of the arteries of the heart with atheroma.
Sometimes a blood clot (thrombosis) forms over a patch of atheroma and completely blocks the blood flow. Depending on the artery affected, this can cause a heart attack, a stroke or other serious problems.
Cardiovascular diseases caused by atheroma
The cardiovascular diseases that can be caused by atheroma include:
Heart disease: The term “Heart disease” is used for conditions caused by narrowing of one or more of the coronary (heart) arteries by atheroma. This can cause angina, heart attack and heart failure. It is common in people over 50 years.
Cerebro-vascular disease – Stroke and TIA: Cerebro-vascular disease means a disease of the arteries in the brain. This can lead to TIA (transient ischemic attack) or a stroke. A stroke means that part of the brain is suddenly damaged. The common cause of stroke is blocking of an artery in the brain by a blood clot which usually forms over some atheroma. A TIA is a disorder caused by temporary lack of blood supply to a part of the brain, resulting in weakness in a part of body. If left untreated it can progress to stroke (paralysis).
Peripheral vascular disease: Peripheral vascular disease is narrowing due to atheroma that affects arteries other than in the heart or brain. The arteries that take blood to the legs are the most affected.
Deep vein thrombosis and pulmonary embolism – blood clots in the leg veins, which can dislodge and move to the heart and lungs.
Risk factors of developing atheroma
Everybody has some risk of developing atheroma. However, certain ‘risk factors’ increase the risk.
Lifestyle risk factors that can be prevented or changed:
- Obesity
- Lack of physical activity (a sedentary lifestyle)
- An unhealthy diet and eating too much salt
- Excessive alcohol intake
- Smoking
Treatable or partly treatable risk factors:
- Hypertension (high blood pressure)
- High cholesterol
- High triglyceride
- Diabetes
- Kidney diseases
- Obstructive Sleep Apnea (OSA)
Fixed risk factors – ones that you cannot alter:
- A strong family history – Individual’s father or brother who developed heart disease or a stroke before they were 55, or an individual’s mother or sister who developed heart disease or a stroke before they were 65
- An early menopause in women
- Age: The older you become, the more likely you are to develop atheroma
If you have a fixed risk factor, you can make extra efforts to tackle any lifestyle risk factors that can be changed.
Assessing your cardiovascular health risk
It is important to detect cardiovascular disease as early as possible so that management with counselling and medicines can begin.
The following people should be assessed to find their cardiovascular health risk:
- All adults aged 40 or more
- Adults of any age who have:
– A strong family history of early cardiovascular disease
– A first degree relative (parent, brother, sister, child) with a serious hereditary lipid disorder
- Obese and Overweight adults having a BMI of 23 or more
- Diabetics
- Hypertensives
- Smokers
- Alcoholics
Knowing about Assessments
A Doctor will –
- Advise a blood test to check your cholesterol and glucose (sugar) level
- Measure your blood pressure and your weight
- Ask you, if you smoke
- Ask, if there is a history of cardiovascular disease in your family. If so, at what age the disease started in the affected family members
A score is calculated based on these factors plus your age and your sex. An adjustment to the score is made for certain other factors such as strong family history and ethnic origin.
Comprehending the assessment score
You are given a score as a % chance. For example, if your score is 30% this means that you have a 30% chance of developing a cardiovascular disease within the next 10 years. This is the same as saying a 30 in 100 chance (or a 3 in 10 chance). In other words, in this example, 3 in 10 people with the same score as yours will develop a cardiovascular disease within the next 10 years.
Note: The score cannot say if you will be one of the three. It cannot predict what will happen to each individual person. It just gives you the odds.
You are said to have a:
High risk – If your score is 20% or more. That is, 2 in 10 chance or more of developing a cardiovascular disease within the next 10 years
Moderate risk – If your score is 10-20%. That is, between 1 in 10 chances
Low risk – If your score is less than 10%. That is, less than 1 in 10 chances
Who should be treated to reduce their cardiovascular health risk?
Treatment to reduce the risk of developing a cardiovascular disease is usually offered to people with:
- Risk assessment score of 20% or more
- An existing cardiovascular disease (to lower the chance of it getting worse or of developing a further disease)
- If you have diabetes, the time that treatment is started to reduce cardiovascular risk depends on factors such as: your age, how long you have had diabetes, your blood pressure and if you have any complications of diabetes.
- Certain kidney disorders
It’s important to know if losing weight will help prevent or improve your condition and its complications
The increased health risk of obesity is most marked when the excess fat is mainly in the abdomen rather than on the hips and thighs. Asians have a high risk for developing diabetes and subsequently heart disease and stroke. A waist measurement of 90 cm or above for (Asian) men and 80 cm or above for (Asian) women is a significant health risk.
There is evidence that even modest weight loss (5–10 %) can reduce cardiovascular disease risk even when the individual remains in the obese range. Few findings from various studies are cited below:
- 5–10 % weight loss showed significant reductions in triglycerides, total cholesterol, and low-density lipoprotein (LDL) cholesterol.
- Those who lost >10 % experienced significantly greater improvements in triglycerides, total cholesterol, and LDL cholesterol than losing less.
- For higher-risk individuals, those who lost 5–10 %, significantly reduced fasting glucose, triglycerides, and total cholesterol; those who lost >10 % improved on all risk factors (except HDL cholesterol) and to a significantly greater degree than those losing less.
- 5 to 10 % weight loss produced improvements in cardiovascular risk factors, but greater weight loss was associated with even greater improvement.
Experts can help you to manage this condition by helping you to lose weight and advising appropriate changes in diet and lifestyle.
Diet plan for clients with/at risk of heart problems focuses on controlling portion size, consumption of fruits & vegetables, whole grains, non- fat dairy products, lean meat, fish and diet low in saturated fat as well as low in sodium and refined carbohydrates.
Once expert guides you on which foods to eat more and which foods to limit, you will be on a disciplined regime aimed towards weight loss and a heart-healthy diet, including regular physical activity and avoiding alcohol.
The right kind of exercise further helps in bringing down the blood pressure, a leading risk factor for CVD. Regular physical activity helps in energy expenditure and also reduces the risk of having a heart attack or stroke.
So don’t hesitate, take a step forward, discuss your medical issues and enjoy a heart – healthy life!